Chest Trauma
Introduction
After head and spinal injury, chest traumais the third most common cause of death.
The major concern with chest traumas is derangements in the flow of air, blood, or both in combination. Chest trauma can be fatal as there are various vital structures in the chest.
Assessment
As soon as the chest trauma patient comes to the hospital, the initial approach towards the patient involves the ABCDEs of trauma. First it is made sure that Airway of the patient is patent and there is no obstruction. Second vital step is to check whether the patient is breathing, third step is to confirm that Circulationof blood is proper, after that to confirm that the patient is neurologically intact (Disability), and finally seeing to it that the patient is completely undressed so the physician can fully assess the patient (Exposure). If any of the above is requirement is lacking, the patient needs resuscitation first.
History and examination can be delayed till resuscitation is done and patient is stable.
A chest injury is any form of physical injury to the chest including the ribs, heart and lungs
History
Brief history can be known from the bystanders, police or close relatives who bring the patient to hospital. The questions should be directed to find out:
1. Previous medical history
2. Any medications being taken
3. History of known allergies
4. Last intake of food
5. Events leading to injury and manner of injury.
The examination in chest trauma depends on the presentation of patient.
The following tests and procedures are performed after the patient is stable
1. X-ray: this is a very important 1st line investigation in blunt trauma which can help to identify many conditions like broken ribs, pneumothorax, hemothorax, injuries to great vessels, and damage to other organs or bones.
2. CT Scan: it is preferred in the hemodynamically stable patient
3. 12 Lead ECG: it can help to diagnose new cardiac abnormalities and arrhythmias.
4. Blood typing and cross-match: it is very essential in case of any trauma if blood transfusion is needed. At least 4 units of blood should be ready in severe cases.
5. Cardiac enzymes: specific chemicals are released into blood after a muscle of heart is damaged. Creatinine Kinase enzyme greater than 200 indicates muscle damage somewhere in the body, but CKMB type of this enzyme indicates cardiac muscle damage. Also, troponin greater than 0.1 indicates heart muscle damage.
6. Coagulation profile: it is typically important if the patient needs blood. It can tell a doctor how well a patient is clotting.
7. Complete blood count: Helps to determine haematocrit and gage the blood loss.
8. Arterial blood gas: Can provide information about lung ventilation and oxygenation as well as acid base status of body.
9. Lactate and Lactic Acid: These enzymes can indicate tissue death or damage.
10. Other: Aortogram, thoracic ultrasound, trans-esophogeal echocardiogram, flexible or rigid esophagoscopy and bronchoscopy are also tests commonly used to investigate the chest trauma patient.
Some serious and life threatening trauma related injuries are worth discussing:
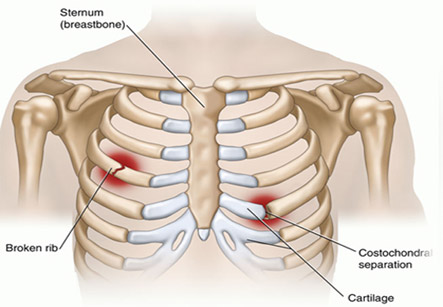
1. Rib Fractures: Pain from fractured rib can be excruciating, and this may cause the patient to take rapid and shallow breaths due to pain. The broken rib may compress the lung causing pulmonary contusion or can puncture the lung causing a pneumothorax. The rib fracture does not have any consequence, and is generally treated with pain relievers.
2. Pulmonary contusions: the most common type of potentially lethal chest trauma. The blunt trauma can tear the capillaries leading toaccumulation of blood in lung tissue. This interferes with gas exchange and causes hypoxia. Contusion canresolve on its own but supplemental oxygen is necessary.However, if there is still breathing insufficiency, intubation and mechanical ventilation may be required.
3. Flail chest: This occurs when several ribs break and the chest wall moves independently of the lungs. It is very painful and almost invariably fatal if not treated immediately.Treatment includes pain killers and positive pressure ventilation.
4. Tension Pneumothorax: This is a more serious complication. In this case, the air continues to exit the lungs into the pleural space, building up pressure in that area. This pressure can compress the superior vena cava.