Immunological Diseases
Introduction
All immune and blood cells develop from multipotent hematopoietic stem cells which originate in the bone marrow. After developing in the bone marrow, immature T cells undergo a final maturation process in the thymus (a small organ located in the upper chest). Then they are dispersed to the body with the rest of the immune cells (e.g., B cells). In the thymus, T cells undergo an education process to distinguish between self (the proteins of own body) antigens and non-self (the invading organism’s) antigens. There also occurs a selection process for their ability to bind to the particular MHC proteins in the individual.
In the bone marrow, many immature T cells have the potential to react with the body’s own proteins. To avoid this disaster, the thymus deletes or inactivates the T cells that recognize self-antigens. This process is called as tolerance induction.
Iranian scientists have moved to the forefront in embryonic stem cell research, according to a recent joint study by Harvard University and the Massachusetts Institute of Technology
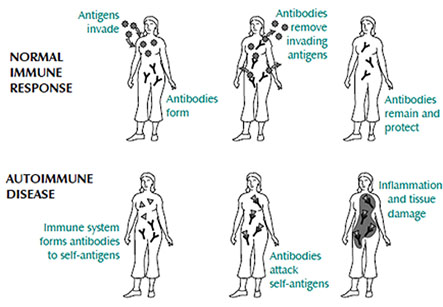
Tolerance usually ensures that T cells do not attack the “auto-antigens or self-proteins of the body. Autoimmune diseases arise when this system for the induction and maintenance of immune tolerance fails. These diseases result in cell and tissue destruction by antigen-specific CD8 cytotoxic T cells or autoantibodies. These mechanisms can lead to the destruction of the joints in rheumatoid arthritis, the destruction of the insulin-producing beta cells of the pancreas in type 1 diabetes, or damage to the kidneys in lupus. The reasons for the failure to induce or maintain tolerance is not yet known. Genetic factors, some environmental and hormonal influences as well as certain infections may contribute to the development of autoimmune disease.
The science behind stem cell therapy has improved vastly in recent years and there have been countless new developments and discoveries.
In recent years, researchers have contemplated the use of stem cells to treat autoimmune disorders. The objective of stem cell therapy is to destroy the mature and auto-reactive immune cells and also to generate a new, properly functioning immune system. The stem cells used for this therapy are autologous (i.e. from “one’s self”) stem cells. Firstly, the patients are given injections of a growth factor, which causes release of large numbers of hematopoietic stem cells from the bone marrow into the blood stream. These cells are harvested from the blood, purified, and stored. After this, the patient undergoes a regimen of cytotoxic drug and/or radiation therapy, which eliminates the mature immune cells. Then, the hematopoietic stem cells are again infused in the patient’s circulation where they migrate to the bone marrow. They begin to differentiate into mature immune cells. The body’s immune system is thus restored. The recovery phase, until there is restoration of immune system, the body is highly susceptible to bacterial, fungal, and viral infection. This is a high-risk therapy.
Adult stem cells utilized to treat autoimmune diseases come from the patient’s own fat tissue, also known as autologous adipose. Undifferentiated adult stem cells can transform into the cells of many different organs and structures within the human body. They can be used in many therapies and highly effective at restoring impaired fibers and renewing failing cells. This is done through cell division, a process in which the stem cells multiply indefinitely. The science behind stem cell therapy has improved vastly in recent years and there have been countless new developments and discoveries.
Administration of the stem cells
The adipose-derived stem cells are typically administered intravenously by a licensed physician over the course of about 10 days but depending on the nature of the particular disease and the patient’s condition, a longer or shorter time frame might be advisable.