Necrotizing Enterocolitis
Introduction
Necrotizing enterocolitis or NEC is one of the conditions occurring in premature infant. This is a gastrointestinal disease which mostly affects premature infants. NEC involves infection and inflammation leading to destruction of the bowel or part of the bowel. NEC is the most common and serious gastrointestinal disorder among hospitalized preterm infants.
NEC usually occurs within the first 2 weeks of life, usually after beginning of milk feeding. At first, feedings are usually given through a tube that goes directly to the baby’s stomach. Premature infants have immature bowels, which are sensitive to changes in blood flow and susceptible to infection.
Causes
The exact cause of NEC is unknown, but one theory is that the intestinal tissues of premature infants are weakened by insufficient oxygen or blood flow. When feedings are started, the added stress of food moving through the intestine allows bacteria normally found in the intestine to invade and damage the intestinal wall. The damage may affect only a short segment of the intestine or can involve a much longer portion.
Iranian specialists have made remarkable achievements in infants' surgeries and Iran is among few countries that have gained access to the latest surgical technologies
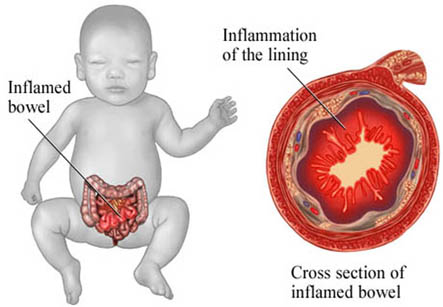
The infant is unable to continue feedings and starts to appear ill if bacteria continue to spread through the wall of the intestines and sometimes into the bloodstream. In severe cases of NEC, a hole or perforation may develop in the intestine, allowing bacteria to leak into the abdomen and cause life-threatening infection.
NEC usually occurs within the first 2 weeks of life, usually after beginning of milk feeding.
Some factors which are thought to increase the risk of developing NEC are the infant formulas, the rate of delivery of the formula, or the immaturity of the mucous membranes in the intestines. Babies who are fed breast milk can also develop NEC, but their risk is lower.
Another theory is that babies born through prolonged difficult deliveries with lowered oxygen levels can develop NEC. Babies with an increased number of red blood cells (polycythemia) in circulation also seem to be at higher risk for NEC.
NEC sometimes seems to occur in epidemics, which means it affects several infants in the same nursery. Although this may occur coincidentally, it suggests the possibility that there may be some cases due to spread from one baby to another.
Signs and Symptoms
The symptoms of NEC can resemble those of other digestive conditions, and may vary from infant to infant. Common symptoms include:
1. Poor tolerance to feedings
2. Poor and prolonged emptying of stomach
3. Decreased bowel sounds
4. Abdominal distension and tenderness
5. Bile-colored (greenish) vomit
6. Diarrhea or constipation
7. Blood in stools
More subtle signs of NEC might include:
1. Apnea (periodic stoppage of breathing)
2. Bradycardia (slow heart rate)
3. Diarrhea
4. Lethargy
5. Fluctuating body temperature.
Advanced cases may show fluid in the abdominal cavity, peritonitis (infection of the membrane lining the abdomen), or shock.
Diagnosis:
The diagnosis of NEC is usually confirmed by the presence of an abnormal gas pattern as seen on an X-ray. There is usually a “bubbly” appearance of gas in the walls of the intestine, large veins of the liver, or the presence of air outside of the intestines in the abdominal cavity. A surgeon may insert a needle into the abdominal cavity to withdraw fluid and to determine whether there is perforation of the intestines.
Treatment
It includes:
• Stopping oral feeds
• Nasogastric drainage (insertion of a tube through the nasal passages down to the stomach to remove air and fluid from the stomach and intestine)
• Intravenous (IV) fluids for fluid replacement and nutrition
• Antibiotics for infection
The baby’s belly size is measured and watched carefully, and periodic blood samples are taken to test for bacteria. Stools are also checked for blood. Sometimes, if the abdomen is so swollen that it interferes with breathing, extra oxygen or mechanically assisted breathing is required to help the baby breathe.
A baby who responds favorably may be back on regular feedings within 72 hours. In most cases, feedings are withheld and antibiotics are continued for 7 to 10 days. In case of bowel perforation, surgery may be indicated.
Severe cases of NEC may require removal of a segment of intestine. Sometimes, if the baby is very ill or there is spillage of stool in the abdomen, the surgeon may require bringing an area of the intestine or bowel to an opening on the abdomen (called asostomy).
Most infants who develop NEC recover fully and do not have further feeding problems. In some cases, scarring and narrowing of the bowel may occur which can cause future intestinal obstruction or blockage.