Trochanteric Fracture
Introduction
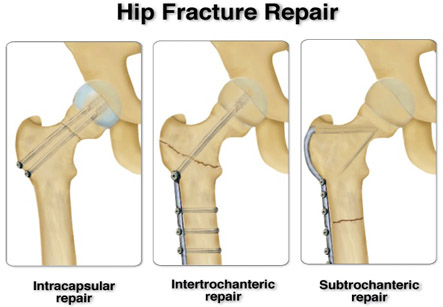
Trochanteric fractures usually occur in older patients, who are more than 65 years old, with greater loss of the bone mass. Conservative methods of treatment are accompanied by the greater percentage of failure as they do not render valid anatomical and functional results. Surgical treatment can be of various types but the use of dynamic implant presents a method of choice in the fixation of the trochanteric fractures. External fixation is also a treatment for this type of fracture. Dynamic implants achieve both dynamisation and compression of the fracture line in the axis of the neck as well as the diaphysis of the femur. This reduces the possibility of mechanical complications, and, at the same time, enables the effective healing of the fracture. Early activation and mobility of the patients is achieved with dynamic method. In patients infected by various diseases and for whom the surgical trauma presents a life threat, the external fixation has to be a method of choice.
Surgical treatment
Standard AP and lateral x-rays of the proximal femur are ordered for evaluation of the fracture. If insertion of an intramedullary device such as the proximal femur nail (PFNA) or trochanter femoral nail (TFN) is planned, imaging of the femoral shaft must be required for measurement of the width of the medullary cavity and also assessment of diaphyseal morphology. If there is excessive anterior bowing of the femur it may be impossible to insert a screw/nail device as the tip of the intramedullary nail might perforate the anterior cortex of the femoral shaft or cause a fracture.
Iran ranks among the top 10 countries in orthopedics and Iranian surgeons perform high quality orthopedic surgeries at highly affordable prices
A full orthopedic and medical assessment of the patient is essential. Surgery should be performed without delay once the patient is considered fit for surgery.
The surgery is performed under regional anesthesia and made to lie in supine position. The fracture is usually treated by closed reduction on operating table under fluoroscopic guidance. This is achieved by longitudinal traction and internal rotation, which usually corrects the deformity. Intraoperative image guidance in two planes is mandatory. The classical approach includes a straight incision on the side of the patient, splitting the iliotibial tract, and gently elevating the vastus lateralis muscle.
Successful treatment of trochanteric fractures requires mechanically stable fixation based on careful planning and the correct use of implants and instruments. Fixation devices have evolved greatly in recent years and many different concepts of fixation provide good results.
Intramedullary fixation is associated with shorter operation time, less blood loss, and earlier mobilization as well as weight bearing. However, this method has not yet proven to be superior to extramedullary fixation of trochanteric fractures.
For stable fractures, the dynamic hip screw (DHS) is the implant of choice. It allows secondary impaction of the fracture along the axis of the gliding hip screw, which must be placed correctly in the centre of the femoral head.
A positioning of DHS in the superior quadrant may lead to failure by cutout of the implant, particularly if the bone is osteoporotic. To avoid incorrect positioning of the DHS, central placement of the guide wire is essential and has to be checked carefully with the use of x-rays in two planes.
For unstable fractures, the dynamic condylar screw and condylar blade plate as well as the DHS in combination with the trochanter stabilizing plate is a valid option for selected cases. . Of the above three methods, the dynamic condylar screw is considered the easiest to insert.
The surgery is performed under regional anesthesia and made to lie in supine position.
Percutaneous insertion of fixation devices for hip fractures has recently been developed. However, in this method, complications such as implant failure and revision surgery appear to occur more often as compared to open hip screw fixations. In cases of pre-existing symptomatic osteoarthritis of the hip in the patient, the trochanteric fracture may be managed by a total hip replacement. Primary arthroplasty in such circumstances is difficult and associated with a high rate of complications. In most of these cases, initial internal fixation is performed. If the patient remains symptomatic after the fracture has healed, an arthroplasty can be performed more easily than in a fresh fracture.