Incise Finger Tendon Sheath
Introduction
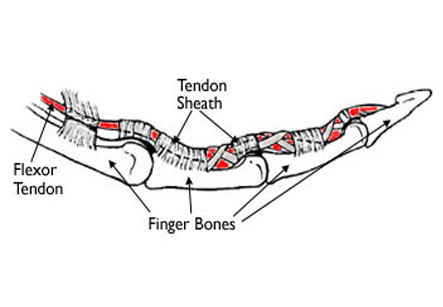
A tendon is a tough band of fibrous tissue which connects muscle to the bone. Tendons are surrounded by specialized tissues known as tendon sheath. This covering protects and helps to nourish the tendons. It also contains blood vessels and nerves too. Sometimes, the sheath can exert pressure on the tendon, limiting movement or causing pain.
In such cases, a surgical procedure which involves incision of a tendon sheath needs to be performed. In this procedure, the tissue surrounding a tendon (tendon sheath or epitenon) is cut. This is necessary to relieve pressure or constriction around a tendon. If the sheath around the tendon is too tight, it can prevent the normal gliding function of the tendon. Incision of the sheath restores function by allowing the tendon to move more freely.
The tendons which control the movements of the fingers pass from the forearm to the wrist and into the hand through a series of tunnels. These tunnels help to hold the tendon close to the bone. If adhesions develop, it can prevent free movement of the tendon.
About 60% and 90% of individuals undergoing flexor tenolysis of the hand show improvement in joint range of motion.
Iran ranks among the top 10 countries in orthopedics and Iranian surgeons perform high quality orthopedic surgeries at highly affordable prices
A tendon sheath incision may also be necessary in the treatment of inflammatory disorders, entrapment disorders, lateral epicondylitis, changes due to fractures and dislocations, or other conditions causing to formation of scar tissue along the tendon. Surgery is recommended when conservative treatments have failed to cause improvement, or when decreased function and pain interfere with daily activities.
In inflammatory disorders such as rheumatoid arthritis, the procedure is most often done in the feet and hands. Entrapment disorders like carpal tunnel syndrome and stenosing tenosynovitis occur mostly in the hands and wrists.
Reason for Procedure
This procedure is used for the purpose of restoring tendon function and to relieve symptoms of loss of function and pain caused by entrapment or compression of the tendon.
Tendons which slide through tight compartments or tunnels such as flexor tendons in hand are most prone to problems with the tendon sheath. The need for tendon release may arise due to conditions such as tenosynovitis, trauma disorders, or fractures and dislocations.
Procedure:
1. This procedure is done under local, regional, or general anesthesia, depending on the location of the involved tendon.
2. The surgery may be performed either endoscopically (by using a special device with camera and miniature instruments) or through an open incision.
3. An incision is made over the tendon. After exploring the sheath and the tendon, the nerves and blood vessels are isolated and protected.
4. Then, the surgeon either cuts away (excises) the sheath entirely or loosens it up (release procedure) by making a cut on one side along its length.
5. Tendon function is evaluated by passive motion, and the wound is closed with sutures.
Prognosis
Successful outcome depends on the indication for the procedure. Restoration of tendon function is mostly achieved, along with relief of pain and swelling. If there are no other complications such as joint contractures, muscle or nerve damage, the procedure should restore normal function. However, the procedure may need to be repeated if the underlying disease process recurs.
About 60% and 90% of individuals undergoing flexor tenolysis of the hand show improvement in joint range of motion. However, some individuals undergoing this surgery find no improvement, and a few even report worsening of symptoms. Also there is small possibility of tendon rupture with this procedure.
Rehabilitation
Rehabilitation therapy after a tendon sheath incision involves exercises and activities specific for the hand. The rehabilitation also depends on degree of injury and the functional limitations. In most cases, a full recovery can be expected after surgery.
Range of motion exercises should be commenced on the adjacent joints as soon as possible, unless there is any contraindication.
The initial therapy is to control swelling using limb elevation, wound care and scar management. Pain may be controlled using local therapies such as cold packs, as needed.
Hand splinting and the advised passive and active range of motion exercises are also initiated after this. The goal of the treatment is restoring full hand function and achieving independence in daily activities.
Return to normal hand function may take up to 3 months. Depending on the location and extent of hand injury, an ergonomist may be called upon to assess working conditions and possible adjustments.