Refractive Surgery
Introduction
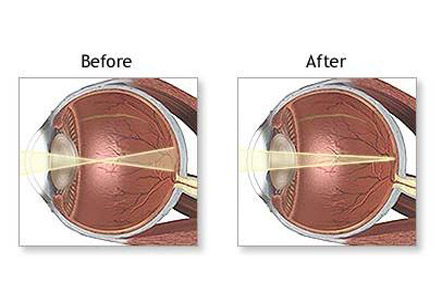
Surgical procedures are now available to permanently eliminate or significantly reduce the need to wear glasses or contact lenses. Even the people with very large refractive errors requiring thick lenses can also be treated. The basic problem in all refractive errors is that the eye cannot focus light rays exactly on the retina. Various refractive surgeries can correct this problem and can reduce or eliminate nearsightedness, farsightedness, and astigmatism. Now it is also possible to reduce the magnitude of severe optical distortion such as spherical aberration. Newly developed intraocular lenses can even correct presbyopia (the reduced ability to focus from far to near occurring in the forties).
There are two basic types of corrective refractive surgery. One type changes the curvature of the cornea (outer surface of the eye). The other changes the internal optics of the eye, either by replacing the natural lens of the eye or by using an intraocular lens in addition to the natural lens.
The refractive surgeries became popular with the advent of radial keratotomy. In this operation, incisions are made in the outer part of the cornea which causes the central part of the cornea to flatten. This corrects mild to moderate degree of nearsightedness. Astigmatism can be corrected with astigmatic keratotomy, in which circumferential incisions are made in the outer part of cornea. Radial keratotomy is not commonly performed now, but astigmatic keratotomy is still performed widely, especially with cataract surgery.
Iran is now ranking first both in the region and in the Middle East and the Iranian ophthalmology science is among the world top majors
For most refractive errors, excimer laser surgery has replaced radial and astigmatic keratotomy because of its ability to remedy precisely a wider range of refractive errors.
The current refractive surgical procedures include:
Photorefractive keratotomy (PRK):
An excimer laser is used to correct low to moderate degrees of farsightedness, nearsightedness, and astigmatism. The thin corneal epithelial layer is removed and some tough underlying tissue is ablated. The final refractive state may not be reached for two or three months. Postoperative haziness of the cornea and cloudy vision used to be common with this procedure, but topical treatment with the drug Mitomycin-C at the time of surgery can prevent such haze.
Laser in-situ epithelial keratomileusis (LASEK):
In this procedure, the outermost corneal layer is treated with dilute alcohol to harden it and is dissected aside. The cornea is reshaped by using excimer laser, and the epithelial layer is then replaced. A newer variation of this procedure is EpiLASIKwhich uses a precise mechanical instrument to push aside the superficial layer of the cornea.
Laser in-situ keratomileusis (LASIK):
An outer flap of the corneal epithelium and supporting tissue is made with the microkeratome and ablation of underlying tissues is made with the excimer laser. As with the above procedures, each laser pulse removes just 0.25 microns of tissue. The results are nearly always predictable and recovery is very rapid. There is no postoperative pain or other discomfort. LASIK is the most commonly performed refractive surgical procedure.
Refractive lens replacement:
In severe cases of farsightedness or nearsightedness, an alternative approach is replacement of the natural lens with an artificial lens of appropriate power. This is essentially the same as cataract surgery. In patients with extremely high refractive errors, it is often the only choice.
Satisfaction with modern refractive surgery is very high, and complications are rare.
Single vision intraocular lenses focus at just one distance. Such lenses can provide an increased range of focus when both eyes are used together. With monovision, near focus with one eye and a distance focus with the other eye can be brought near to reduce dependence on glasses. However the recent developments in intraocular lenses can actually change position and shape to provide a clear focus at different distances. It utilizes the natural focusing muscle (ciliary muscle) of the eye to provide a continuous focus from far to near.
Phakic intraocular lens implantation:
A special intraocular lens is placed either in front of or behind the iris so that it works with the natural lens to bend the light rays more appropriately. This type of lens implant is particularly beneficial to younger patients with high myopia. Some uncommon problems, such as cataract formation, have been reported.
Risks involved:
1. In corneal procedures:
• Flare around lights at night
• Undercorrection or overcorrection
• Need of revision procedure.
2. In LASIK
• Improper cutting of the corneal flap leading to corneal irregularity.
• The excimer laser ablation can be off-center, resulting in reduced vision, halos around lights, and astigmatism.
3. In lens exchange surgery, infection, bleeding, and retinal detachment can occur.
Satisfaction with modern refractive surgery is very high, and complications are rare. Even so, the risk involved may not justify the use of surgery if adequate vision and comfort can be achieved with eyeglasses or contact lenses.