Deep Brain Stimulation for Parkinson’s
Introduction
Parkinson’s disease is a severe degenerative disease of the brain. It mainly occurs due to a slow loss of a specific type of nerve cell, located in an area of the brain called the substantia nigra. These dopaminergic nerves are responsible for the production of a natural chemical called dopamine. Deficiency of this chemical in the brain may lead to tremors, difficulty in movement, posture maintenance, etc. At late stages it may also lead to complete immobility. There are numerous drugs that are used to treat Parkinson’s disease. These drugs mainly act by increasing the production of dopamine in brain. Many of these drugs are associated with side effects. Additionally over time most of these drugs lose their efficacy when used over a long period of time. As of now there is no cure for Parkinson’s disease. Deep brain stimulation is an option for treatment of Parkinson’s disease. Deep Brain Stimulation of the thalamus was approved by the FDA for the treatment of Parkinson’s disease and essential tremor in 1997.
Surgical Procedure
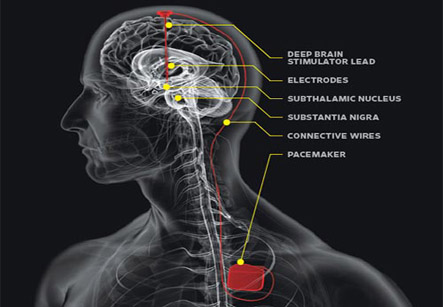
Basically this method involves placement of electrodes in an area of the brain called the thalamus or globus pallidus. The electrodes are then connected by wires to a type of pacemaker device or impulse generator that is surgically placed under the skin over the chest just below the collar bone. Once the device is switched on it sends continuous electrical pulses to the target areas in the brain, blocking the impulses that cause tremors. The impulse generators are programmed and controlled with devices or magnets to generate desired signals to the electrodes in the brain. The device usually lasts for around three to five years.
Iran has made significant progress in neurosurgery and The world renowned Iranian scientist in neurological surgery Professor Majid Samii has garnered the 2014 Golden Neuron Award. We have all the information you need about public and private clinics and hospitals that provide Neurosurgical surgeries in Iran, Islamic Republic Of with the best quality and lowest possible price
The exact location of the electrode is found out by performing CT scans and MRI scans.
The surgery per se is basically divided into two parts. The first part involves opening up of the affected parts of the brain. The area of the operation is delineated over shaved and cleaned scalp and an incision is made under general anesthesia. The skull is drilled and a bone flap is removed to expose the brain. Surgical tools are used to place one or more non-activated electrode at the site of the disease. The exact location of the electrode is found out by performing CT scans and MRI scans. The loose ends are placed underneath the skin of the head and the incision is closed with sutures.
The second part of the operation involves placement of the impulse generator under the skin under the collar bone. Once in place the impulse generator is activated. This part of the operation usually takes place a week after the first part.
Post operative considerations
Usually recovery from the operation is uncomplicated. Around a week of hospital stay may be needed. The head end of the bed is usually kept raised to help reduce swelling of head and face. Medications are usually prescribed to alleviate pain.
Patient is advised bed rest for two weeks after deep brain stimulation surgery. Heavy activities are forbidden for four to six weeks after surgery. This includes jogging, swimming, or any physical education classes.
Common complications include those due to anesthesia that include allergies to the anesthetic agents, problems of breathing etc. Other risks include problems with memory, speech, hearing, sight, movement, muscle weakness, balance, muscle co-ordination and other functions. The chance of these complications is low at 2-3% approximately. Sometimes patients may develop bleeding, stroke, coma, seizures, infections and swelling of the brain after brain surgery. These are serious complications that need immediate management.
Studies have shown that deep brain stimulation at the thalamus reduces the tremors and other disease symptoms like rigidity, slowness of movement, stiffness, and walking concerns in almost 70% of the patients.
Patients with an electrode may be warned of activation or discomfort around some electrical devices. Theft detectors and screening devices, like those found in airports, department stores and public libraries, can cause the neurotransmitter to switch on or off. Usually, this only causes an uncomfortable sensation but sometimes symptoms may worsen. Most patients are given a magnet to modulate their device. This magnet is usually very powerful and can damage electrical devices such as the computer, cell phone, television or credit cards.