Thyroidectomy
Introduction
Thyroidectomy is the surgical removal of all or part of the thyroid gland. This gland is situated in the neck. It produces thyroxin hormones that regulate metabolism. The surgery may be of following types:
1. Total or near-total thyroidectomy—all of the thyroid gland is removed
2. Thyroid lobectomy or partial thyroidectomy—removal of only a part of the thyroid (the right or left lobe or the isthmus connecting the two lobes)
Indications:
All or part of the thyroid gland may be surgically removed for any of the following reasons:
• Overactive thyroid (hyperthyroidism) due to Grave’s disease or an over-functioning thyroid nodule
Surgeons often perform a thyroidectomy when a patient has thyroid cancer or some other condition of the thyroid gland (such as hyperthyroidism) or goiter
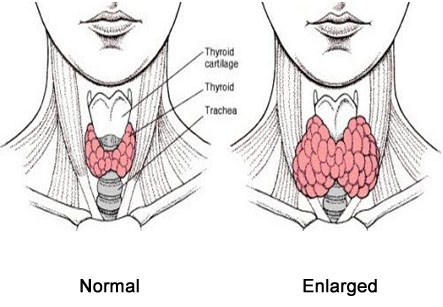
• Enlarged thyroid gland (goiter) causing significant symptoms
• Thyroid nodule(s) which are suspicious of harboring cancer
• Thyroid cancer
Possible Complications:
Complications are rare, but no procedure is completely free of risk. These may include:
• Damage to the parathyroid gland, which controls calcium metabolism (this can result in nerve and heart problems)
• Voice changes due to damage to nerves leading to the voice box (very rare)
• Scarring
• Bleeding
• Infection
• Thyrotoxic crisis (sudden excessive release of thyroid hormone at toxic levels which is very rare)
Some factors that may increase the risk of complications include:
• Severity of hyperthyroidism
• Size of goiter
• Smoking
• Obesity
• Alcoholism
• Poor nutrition
• Long-term illness
Before the procedure:
The doctor may do the following:
• Physical exam
• Laboratory and/or imaging tests to assess thyroid function and anatomy, such as:
• Ultrasound — this uses sound waves to evaluate organs in the body
• MRI —uses magnetic waves to produce images of the inside of the body
• Thyroid medicines to suppress thyroid activity in patients with hyperthyroidism before surgery
• Thyroid scan—uses a radioactive substance and scanning tool to evaluate the thyroid gland
Leading up to your procedure:
Talk to the doctor about the medicines. Patient is asked to stop taking some medicines up to one week before the procedure, such as:
• Aspirin or other anti-inflammatory drugs
• Blood thinners, such as clopidogrel or warfarin
• Patient should not eat or drink anything after midnight the evening before the procedure.
• Arrange a relative or friend for transportation to and from the hospital.
This surgery is done under general anesthesia which means the patient is asleep and there is no pain during the procedure.
Procedure
An incision is made in the front of the neck. Bleeding vessels are clamped and tied off. All or part of the thyroid gland is cut away or separated from other tissues in the neck. Care is taken to avoid injury to other nearby glands and nerves. Bleeding is controlled with special tools that compress and seal the torn ends of the vessels. The incision is closed with stitches. The edges of skin are stitched together. A drain is often left in overnight which helps to drain any extra fluids.
Patient may feel discomfort in the neck for several days. The pain can be treated with medicines.
The thyroid gland is removed to treat thyroid cancer. In this case, lymph nodes in the area are also removed. This will test if the cancer has spread.
This surgery takes about 2-4 hours for completion.
Anesthesia prevents pain during the procedure. However, pain after the procedure is very common. Patient is given medicine to help manage this.
Average Hospital Stay
The usual length of stay in hospital is one day. The doctor may choose to extend the stay if any complications arise.
Post-procedure Care
At the Hospital
Patient may feel discomfort in the neck for several days. The pain can be treated with medicines.
In some cases, patient may have a hoarse voice for a few days.
Depending on how much of the thyroid is removed, patient often needs to take replacement thyroid hormone.
In some cases of thyroid cancer, patient may require radioactive iodine treatments. This is called as remnant ablation.
At Home
After returning home, following steps need to be taken to ensure a smooth recovery:
Keep the incision clean and dry.
Do not apply make-up or lotions to the incision area.
Do not get the incision wet until the doctor allows. If it does get wet, dry it immediately.
Perform neck exercises as instructed by the doctor.
Take all medicines exactly as prescribed by the doctor.
Be sure to schedule follow-up visits with the doctor.