Intracytoplasmic Sperm Injection ICSI
Introduction
Intracytoplasmic sperm injection (ICSI) is used as part of an in vitro fertilization (IVF) technique to help the infertile couples to conceive a child. ICSI is used in about half of the IVF treatments and it is considered as the most successful form of treatment for male factor of infertility. In this technique, only one sperm is required and it is injected directly into the female egg or ovum. The fertilized egg (embryo) is then transferred to the uterus (womb).
During ICSI, the sperm need not travel to the egg or penetrate the outer layers of the egg. Therefore, this can help the infertile couples in whom where the man’s sperm cannot reach to the egg or cannot fertilize the egg for some reason even after reaching.
Indications of ICSI:
This method is recommended for couples if the male partner has:
1. A very low or zero sperm count.
2. A high percentage of morphologically abnormal sperm. This can lead to poor motility and inability to reach the egg.
Iran ranks first in the region in terms of infertility treatment studies
3. Sperm that cannot be ejaculated but can be collected from the testicles or from the duct where sperm is stored (epididymis). This is done in case of male partner having an irreversible vasectomy or injury.
4. Problems with getting an erection and also with ejaculation, which can happen due to spinal cord injuries or diabetes.
It can also be done if enough eggs could not be retrieved in IVF cycle or if eggs retrieved for IVF failed to be fertilized.
The procedure:
As with any IVF treatment, the woman is given fertility medications to stimulate the ovaries to develop several mature eggs suitable for fertilization. When the eggs are ready for retrieval, the patient and the partner need to undergo separate procedures.
The partner may produce a sperm sample himself by ejaculating into a sterile cup on the same day as that of egg collection. If there is no sperm in the semen, doctors can extract sperm from under local anesthetic. It can be done by two methods.
1. The doctor can extract the sperms by using fine needle from the Epididymis and this procedure is known as percutaneous epididymal sperm aspiration (PESA)
2. They can also be retrieved from the testicle, in a procedure known as testicular sperm aspiration (TESA).
3. Another technique involves a biopsy of testicular tissue, which sometimes has sperms attached. This is called testicular sperm extraction (TESE) or micro-TESE, if the procedure is carried out with a microscope. This procedure can also be carried out some time before the treatment cycle begins, and under local anesthesia. The retrieved sperms at that time are frozen and used in current cycle. It causes minimal discomfort and can be relieved with regular painkillers.
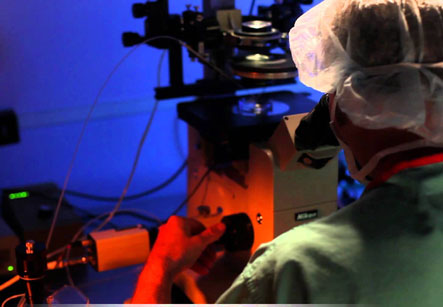
After this, the eggs are removed from the woman under a local anesthetic using a fine, hollow needle. This process can be guided by an ultrasound which helps the doctor to locate the eggs. The individual sperms are isolated by an embryologist in the lab and are injected directly into the individual eggs. Two days later the fertilized eggs divide and multiply to become clumps of cells called as embryos.
After this, the doctor transfers one or two embryos into the uterus through the cervix using a thin catheter as in a standard IVF procedure.
Embryos are usually transferred two to three days after fertilization, or five days after fertilization in blastocyst stage.
If the patient is under 40 years of age, one or two embryos are transferred. If age is 40 or above, a maximum of three embryos are transferred in case of using own eggs, or two in case of using donor eggs. Extra embryos remaining after the cycle are frozen in case this cycle does not succeed to pregnancy.
Embryos are usually transferred two to three days after fertilization, or five days after fertilization in blastocyst stage. If the patient desires to transfer only one embryo, called as elective single embryo transfer, or eSET, a blastocyst transfer is preferred as it can improve the chances of a successful pregnancy and also a healthy, single baby.
If all process goes well, an embryo attaches to the uterus wall and continues to grow to become a single baby. This can be confirmed by a pregnancy test performed after about two weeks of embryo transfer.